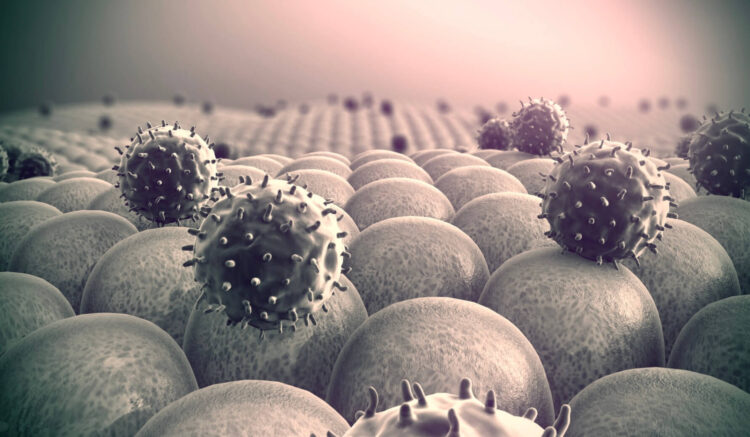
The excessive or inappropriate use of antibiotics in human medicine, veterinary practice, and agriculture has accelerated the development of resistant infections. Bacterial resistance to antibiotics poses a global public health threat. The rise of resistant bacteria is leading to a situation where common infections that were once easily curable could become untreatable. In fact, antibiotic resistance is contributing to an increase in morbidity and mortality. It is estimated that by 2050, the epidemic of bacterial resistance will be responsible for 10 million deaths annually, causing more deaths from resistant infections than from cancer.

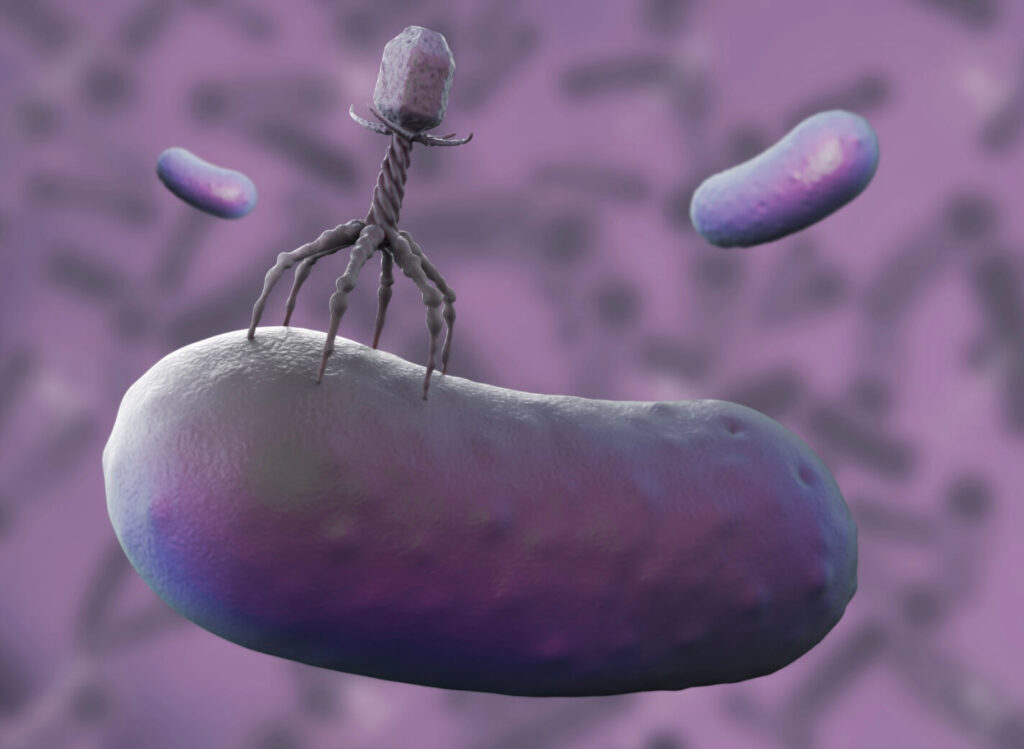
Amid this crisis, bacteriophages emerge as a promising hope. Their ability to target specific bacteria, adapt to mutations, and their potential to offer personalized therapies are qualities that could revolutionize the treatment of resistant infections.
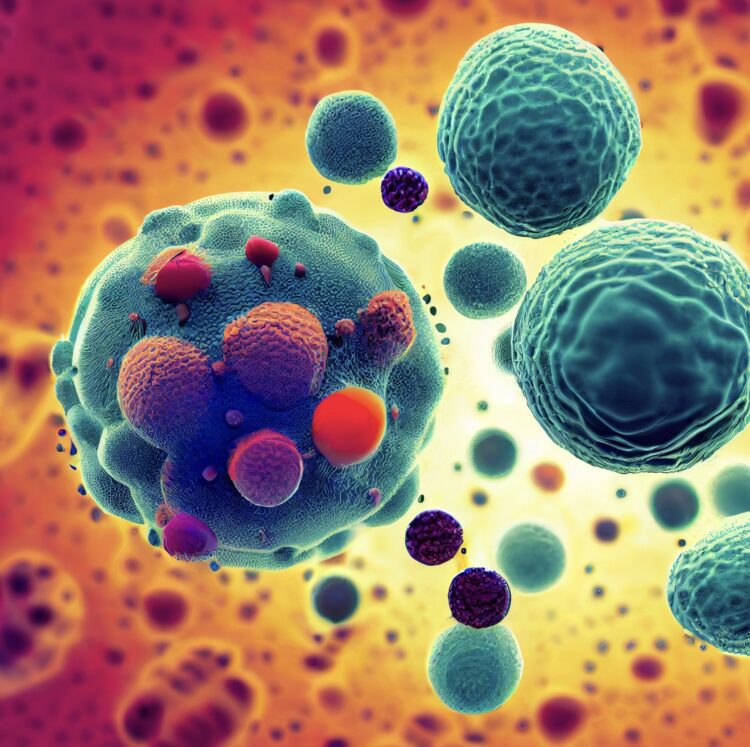
Bacteriophages, or phages, are viruses capable of infecting specific bacteria and replicating within them. These viruses have a simple yet powerful structure: they consist of genetic material surrounded by a protein capsid that selectively adheres to certain bacteria. Once the phage binds to the host bacteria, it injects its genetic material and uses the bacterial cell machinery to replicate, eventually leading to the death of the host (bacterial lysis) and the release of new phages to continue the cycle.
In this way, phages are being used to treat bacterial infections that are resistant to multiple antibiotics, offering hope for patients with previously untreatable diseases. Additionally, they are used in cleaning and disinfection applications, for example, in the food industry and hospitals, to combat resistant bacteria and prevent infections. In some cases, combined therapies of phages and antibiotics are being explored to increase effectiveness and reduce the emergence of resistance.
On the other hand, phages are highly specific and selective. Each type of phage attacks a particular species of bacteria, reducing the impact on the body’s normal microbiota, avoiding collateral damage to other beneficial bacteria. Moreover, their ability to rapidly evolve to adapt to bacterial mutations allows them to maintain their effectiveness even against bacteria that develop resistance.
Thus, the ability to specifically target pathogenic bacteria, their lower toxicity, and their potential to evolve make them an invaluable tool in the search for effective solutions to combat bacterial infections in an increasingly challenging world in terms of antibiotic resistance.